Can Advanced Glycation End Products Be Removed From Skin
- Original investigation
- Open Access
- Published:
Avant-garde glycation end-products, measured as skin autofluorescence, associate with vascular stiffness in diabetic, pre-diabetic and normoglycemic individuals: a cross-sectional study
Cardiovascular Diabetology volume 20, Article number:110 (2021) Cite this article
Abstract
Background
Avant-garde glycation end-products are proteins that become glycated later on contact with sugars and are implicated in endothelial dysfunction and arterial stiffening. We aimed to investigate the relationships betwixt avant-garde glycation cease-products, measured as skin autofluorescence, and vascular stiffness in diverse glycemic strata.
Methods
We performed a cross-exclusive analysis within the European Prospective Investigation into Cancer and Nutrition (EPIC)-Potsdam cohort, comprising n = 3535 participants (median historic period 67 years, 60% women). Advanced glycation end-products were measured every bit skin autofluorescence with AGE-Reader™, vascular stiffness was measured equally pulse wave velocity, augmentation alphabetize and ankle-brachial alphabetize with Vascular Explorer™. A subset of 1348 participants underwent an oral glucose tolerance examination. Participants were sub-phenotyped into normoglycemic, prediabetes and diabetes groups. Associations betwixt skin autofluorescence and various indices of vascular stiffness were assessed by multivariable regression analyses and were adjusted for age, sex, measures of adiposity and lifestyle, blood pressure, prevalent conditions, medication use and claret biomarkers.
Results
Skin autofluorescence associated with pulse wave velocity, augmentation index and talocrural joint-brachial index, adjusted beta coefficients (95% CI) per unit skin autofluorescence increase: 0.38 (0.21; 0.55) for carotid-femoral pulse wave velocity, 0.25 (0.14; 0.37) for aortic pulse wave velocity, i.00 (0.29; i.70) for aortic augmentation alphabetize, 4.12 (2.24; 6.00) for brachial augmentation index and − 0.04 (− 0.05; − 0.02) for ankle-brachial alphabetize. The associations were strongest in men, younger individuals and were consistent across all glycemic strata: for carotid-femoral pulse moving ridge velocity 0.36 (0.12; 0.60) in normoglycemic, 0.33 (− 0.01; 0.67) in prediabetes and 0.45 (0.09; 0.fourscore) in diabetes groups; with similar estimates for aortic pulse wave velocity. Augmentation index was associated with skin autofluorescence only in normoglycemic and diabetes groups. Talocrural joint-brachial index inversely associated with skin autofluorescence beyond all sexual activity, age and glycemic strata.
Conclusions
Our findings betoken that avant-garde glycation end-products measured as skin autofluorescence might exist involved in vascular stiffening independent of age and other cardiometabolic risk factors not just in individuals with diabetes but too in normoglycemic and prediabetic conditions. Pare autofluorescence might prove as a rapid and non-invasive method for assessment of macrovascular disease progression across all glycemic strata.
Groundwork
Vascular stiffness is a pathophysiological process involving endothelial and vascular smooth muscle cells (VSMCs), extracellular matrix (ECM), perivascular adipose tissue and other integral components of the vascular wall [1]. Arterial stiffness independently predicts cardiovascular risk, causing isolated systolic hypertension and excessive penetration of pulse pressure into the microvasculature of target organs that operate at low vascular resistance, contributing to end-organ damage, and promoting left ventricular remodeling, dysfunction, and failure [2]. The underlying mechanisms of vascular stiffness are all the same incompletely understood, but accumulating bear witness supports the involvement of pathogenic factors such as advanced glycation end-products (AGE) in its pathogenesis [three]. AGE are stable compounds that accumulate on long-lived proteins; they are formed past the reaction of proteins or lipids with aldose sugars and farther molecular rearrangements. Age germination is accelerated in hyperglycemia, renal failure, and inflammatory conditions [iii]. Historic period promote and exacerbate endothelial dysfunction [4] and functional arterial stiffening by reducing the phosphorylation status and expression of endothelial nitric oxide synthase (eNOS) [iii, 5]. Moreover, AGE take been linked to structural arterial stiffening via crosslinking the collagen and elastin molecules, which results in an increase in the ECM expanse and VSMC phenotypic changes [3, 6]. AGE also activate Toll-like receptor four/NF-κ light-concatenation enhancer of activated B cells (NF-κB) [three, 7], which contributes to the development of vascular inflammation. In contempo years, peel autofluorescence (AF) emerged every bit a not-invasive marker of AGE accumulation in the skin tissue [8,9,10].
Human studies examining the associations betwixt AGE and arterial stiffness focused primarily on high-risk patients with chronic disease, such as hypertension [11], end-stage renal disease [12], diabetes type 1 [thirteen] and type 2 [ix, 14]. As of at present, the relationships between AGE and vascular stiffness in persons without cardiometabolic affliction are equivocal [ix, fifteen, 16]. There is likewise a paucity of insight in the interrelationships of AGE with glucose and HbA1c levels relating to vascular stiffness. Vascular stiffness have been shown to increase with higher HbA1c and glucose levels in diabetes patients [17, 18], however, the findings in normoglycemic persons are inconsistent [xviii, 19].
We hypothesized that Age measured as pare AF are associated with vascular stiffness across all glycemic strata, and investigated these relationships in a cantankerous-sectional sub-study (Epic-DZD) nested within the population-based European Prospective Investigations into Cancer and Diet (Epic) Potsdam cohort.
Methods
Report design and participants
We performed a cantankerous-sectional analysis inside the European Prospective Investigation into Cancer and Diet (EPIC) Potsdam Study, a population-based unselected longitudinal cohort from the municipality of Potsdam, Deutschland. At baseline, approx. 27,500 men and women were recruited between 1994 and 1998 [20]. Participants are followed up via questionnaires regarding incident diseases, all-crusade mortality, dietary patterns, physical activity status, lifestyle and anthropometric measures. Of those participants who responded to the sixth wave of follow-upward questionnaires betwixt 2014 and 2016 (n = 15,424), n = 8517 were invited for a concrete examination betwixt 2014 and 2020 to collect data on nutritional and cardiovascular phenotyping and to place take chances factors for development and progression of chronic diseases, such as type 2 diabetes mellitus. Until 31 January 2020, 4370 participants were examined. The belittling sample comprised 3535 participants with available peel AF and vascular stiffness measurements, Boosted file 1: Figure S1. All examinations were performed in quiet and temperature-controlled rooms by trained study nurses using standardized protocols. The study was conducted co-ordinate to the Annunciation of Helsinki and approved by the Ethical Committee of the State of Brandenburg, Deutschland. All participants provided written informed consent.
Measurements of AGE
Age accumulation in the skin was estimated with peel autofluorescence every bit measured with AGE-Reader (DiagnOptics Technologies B.5., Version SU 2.four.2.ii, Groningen, Kingdom of the netherlands). The technical description of the measurement is provided elsewhere [eight, 9]. Skin AF was measured in seated position on the inner side of the right forearm below the elbow fold in 3 consecutive measurements, every bit described past the manufacturer. The hateful of 3 measurements was used in the analyses. If a participant had tattoos, pigmentation, wounds or scars on the right forearm, measurements on the left forearm were performed instead.
Measurements of vascular stiffness
Parameters of vascular stiffness (carotid-femoral and aortic pulse wave velocities [cfPWV and aoPWV], brachial and aortic augmentation indices [brAIx and aoAIx], ankle-brachial index [ABI]) were recorded and calculated by Vascular Explorer software (Enverdis GmbH, Jena, Germany). Vascular Explorer implements single-point, suprasystolic brachial oscillometry pulse wave analysis for the assessment of PWV and AIx, was validated against other oscillometric, photoplethysmographic and Doppler devices and deemed feasible in epidemiologic studies [21, 22]. Measurements were performed with appropriate arm and leg cuffs after at to the lowest degree 10 min resting in supine position. Pulse wave analysis, ankle and brachial blood pressures were automatically computed by software mediated analysis of photoplethysmographic signals from finger and toe and volume changes in the inflatable cuffs. The ABI was calculated by the software using the blood pressure readings in the lower and upper extremities. Participants were asked to refrain from speaking and advised to exhale calmly during the measurements. Exclusion criteria for this examination were amputations of limbs, open up wounds at measurement sites, dialysis shunts, paralyses, lymph edema on artillery or legs, bandages, or anti-embolism compression stockings which could not be removed.
Measurements of glycemic and other laboratory parameters
Low-density lipoprotein (LDL), high-density lipoprotein (HDL) and full cholesterol, triglycerides and C-reactive protein (CRP) were measured in serum, HbA1c in plasma EDTA. Blood samples were taken at random and immediately processed for further analyses. A three-point oral glucose tolerance exam (OGTT) was performed on a subset of fasting participants (n = 1348). Exclusion criteria for OGTT were established diabetes, antidiabetic treatment, fasting plasma glucose (FPG) < 3.9 mmol/l or ≥ 11.1 mmol/50, or participant's unwillingness to undergo the OGTT process. Participants were offered a 75 g oral glucose load, and fasting besides as 2-h plasma glucose concentrations were determined. All laboratory analyses were performed at the Establish for Medical Diagnostics Berlin-Potsdam using automated, standardized and quality-controlled assays.
Statistical analyses
Characteristics of the written report participants were evaluated according to the quintiles of skin AF. Missing data were not imputed, participants with missing data were excluded listwise. Right-skewed concentrations of HbA1c, triglycerides and CRP were normalized by log-transformation prior to whatsoever analyses. For associations between skin AF and vascular stiffness, linear and logistic multivariable regressions were constructed. Model 1 was adjusted for sexual practice and age, model 2 was additionally adjusted for BMI, waist circumference, smoking status (three categories: non-smoker, former smoker, current smoker), recreational concrete activity (biking and sports, h/week), systolic and diastolic blood pressure, pulse, prevalent atmospheric condition (prevalent heart failure, prior myocardial infarction or stroke), antihypertensive and lipid-lowering handling, CRP, LDL-, HDL- and total cholesterol, triglycerides and HbA1c. Interactions were evaluated on multiplicative scale by creating cantankerous production terms and assessing the blastoff level. For the stratified analyses, abdominal adiposity was divers using sex-specific clinical cut-offs: in men > 102 cm, in women > 88 cm. In improver to the analyses on continuous measures of vascular stiffness, we defined vascular stiffness by two thresholds—cfPWV ≥ 10 g/s and cfPWV ≥ 12 m/southward—as recommended past the ESC guidelines [23, 24]. The shape of association between peel AF with vascular stiffness was evaluated with restricted cubic splines with iii knots at 5th, 50th and 95th percentiles. Median peel AF was used as the reference, non-linear trend in the splines was assessed with the Wald test.
Further, we evaluated whether the relationships betwixt peel AF and vascular stiffness were modified by glycemic status. To this finish, we categorized the participants according to their HbA1c level and use of antidiabetic drugs in iii groups: normoglycemic (HbA1c < 5.7% and no antidiabetic treatment), prediabetes (vi.five% > HbA1c ≥ 5.seven% and no antidiabetic treatment), diabetes (HbA1c ≥ six.five% or prevalent diabetes at Epic-Potsdam baseline, or antidiabetic handling), Additional file 1: Figure S1. In participants with available OGTT (due north = 1348) we farther characterized the prediabetes group based on several aspects of impaired glucose metabolism, such equally dumb fasting glucose (IFG: 7 mmol/50 > FPG ≥ 5.6 mmol/l), impaired glucose tolerance (IGT: xi.1 mmol/50 > two h plasma glucose ≥ vii.8 mmol/l), abnormal HbA1c (six.5% > HbA1c ≥ five.vii%) or any abnormal glycemic value (IFG or IGT or abnormal HbA1c), Additional File 1: Figure S1.
A two-sided p < 0.05 denoted statistical significance. All statistical analyses were performed using SAS (Version 9.4, Enterprise Guide 7.one, SAS Constitute Inc., Cary, NC, U.s.a.).
Results
Characteristics of written report participants
Participants' characteristics according to the quintiles of pare AF are shown in Table i. Participants with higher skin AF values were on average older, more likely to exist men, had higher BMI, waist circumference and blood force per unit area. The fraction of smokers, hypertensive individuals, participants with CVD, and individuals on antihypertensive, antidiabetic and lipid-lowering drugs increased across skin AF quintiles. Concentrations of CRP, triglycerides and creatinine also increased with higher skin AF, while LDL-, HDL- and total cholesterol decreased beyond skin AF quintiles. In unadjusted analyses, skin AF positively correlated with HbA1c, Fig. 1a and increased linearly across all glycemic strata, p < 0.0001 for tendency, Fig. 1b. The median skin AF (IQR) was 2.17 (i.89–two.48) for normoglycemic, 2.22 (ane.96–ii.54) for prediabetes, ii.47 (1.14–2.85) for diabetes groups.
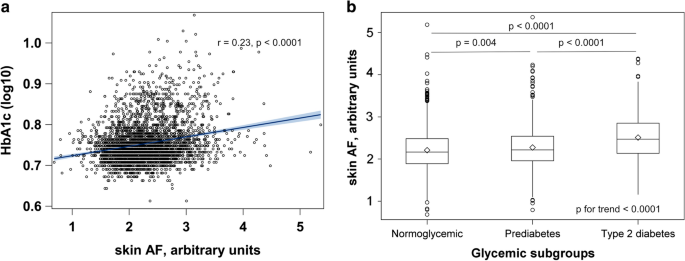
Associations between skin AF and glycemic status in the Epic-DZD written report. North = 3535. Glycemic status was defined as follows: normoglycemic (HbA1c < 5.7% and no antidiabetic treatment), prediabetes (6.five% > HbA1c ≥ 5.7% and no antidiabetic handling), diabetes (antidiabetic treatment, HbA1c ≥ vi.5% or prevalent diabetes at Ballsy-Potsdam baseline). Differences in medians of pare AF were compared with 1-fashion ANOVA with Tukey–Kramer's correction for multiple testing. Linear trend in peel AF across glycemic strata was assessed with linear regression. AF autofluorescence, HbA 1c glycated hemoglobin 1C
Relationships between skin AF and vascular stiffness in the Ballsy-DZD study, n = 3535
In the adjusted models, skin AF positively associated with PWV, AIx and negatively with ABI, Table 2. In a comparative analysis with standardized beta coefficients, peel AF showed a stronger association with PWV and ABI than many other classic cardiometabolic risk factors, including age, waist circumference, HbA1c and CRP, Additional file 1: Table S1. In its relation to AIx, issue estimates of pare AF were higher than those of HbA1c, CRP, cholesterol, triglycerides, Additional file i: Table S1.
Considering there was evidence for statistically significant interactions of skin AF with sex and historic period in relation to PWV and AIx, all analyses were stratified by sex and median age (67 years), Fig. two. Stratified analyses revealed that the associations betwixt skin AF and PWV, AIx were nowadays only in men. One unit increase in skin AF was associated with 0.63 (95% CI 0.38; 0.89) 1000/s increase in cfPWV in men compared with 0.sixteen (− 0.06; 0.39) in women, with similar estimates for aoPWV, Fig. 2a. For aoAIx, the estimates were 1.98 (0.89; iii.07) in men and 0.02 (− 0.92; 0.96) in women, with a similar pattern for brAIx, Fig. 2b. Moreover, when stratified for median age, the associations between peel AF and vascular stiffness were markedly stronger in individuals < 67 years (for instance, cfPWV: 0.41 (0.xiv; 0.68) compared with 0.15 (− 0.07; 0.37) in individuals ≥ 67 years, brAIx: 3.53 (0.20; vi.86) compared with − 0.95 (− 3.36; one.46)), Fig. 2a, b. Even though there was a significant interaction betwixt pare AF and waist circumference (p = 0.02), the effect estimates in leaner individuals and individuals with abdominal adiposity were consistent, Fig. 2a, b. When we examined the relationships between pare AF and PWV beyond categories of glycemic strata defined past HbA1c levels and antidiabetic treatment, the effect estimates were consequent across all glycemic strata: for cfPWV 0.36 (0.12; 0.60) in normoglycemic, 0.33 (− 0.01; 0.67) in prediabetes and 0.45 (0.09; 0.fourscore) in diabetes groups; a similar direction was observed for aoPWV. AIx was associated with skin AF only in normoglycemic (1.03 (0.008; 2.05) for aoAIx and 5.xiv (two.52; vii.76) for brAIx) and diabetes groups (i.72 (0.23; 3.22) for aoAIx and 5.00 (0.79; 9.22) for brAIx), but non in prediabetes group, Fig. 2a, b. ABI inversely associated with skin AF across all sexual activity, historic period, obesity and glycemic strata, though stronger associations were present in men and younger individuals (Fig. 2c).
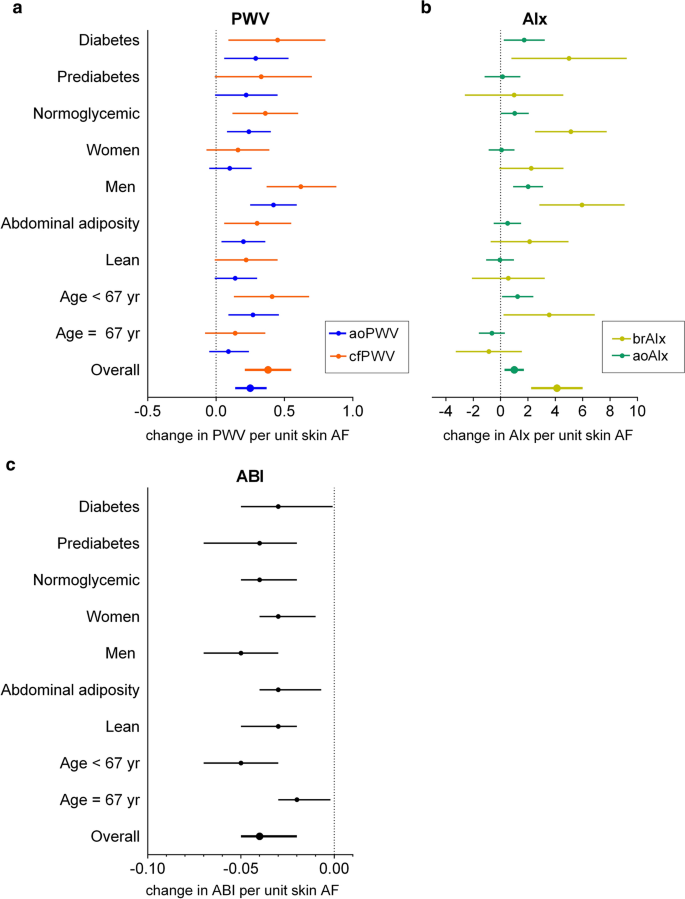
Adapted associations between skin AF and vascular stiffness in the Ballsy-DZD written report. Adapted associations between skin AF and parameters of vascular stiffness (a PWV, b AIx, c ABI) in the Epic-DZD written report, stratified by sex, median historic period, intestinal adiposity and glycemic status. Changes in vascular stiffness are per 1 unit increase in peel AF. Analyses were performed on fully adjusted model ii. p values for interaction terms: cfPWV: skin AF with sex, p = 0.002, with age, p = 0.07, with waist circumference, p = 0.02, with glycemic status, p = 0.77; aoPWV: pare AF with sex, p = 0.002, with age, p = 0.07, with waist circumference, p = 0.02, with glycemic status, p = 0.78; aoAIx: skin AF with sex, p = 0.0008, with historic period, p = 0.001, with waist circumference, p = 0.44, with glycemic status, p = 0.99; brAIx with sex, p = 0.006, with age, p = 0.004, with waist circumference, p = 0.67, with glycemic status, p = 0.37; ABI: skin AF with sexual activity, p = 0.10, with age, p = 0.01, with waist circumference, p = 0.forty, with glycemic status, p = 0.58. Analyses were adjusted for sex activity and age, BMI, waist circumference, smoking status (three categories: non-smoker, former smoker, current smoker), recreational physical activity (biking and sports, h/week), systolic and diastolic blood pressure, pulse, prevalent conditions (prevalent heart failure, prior myocardial infarction or stroke), antihypertensive and lipid-lowering treatment, CRP, LDL-, HDL- and total cholesterol, triglycerides and HbA1c. EPIC-DZD Sub-study of European Prospective Investigations into Cancer and Nutrition, AF autofluorescence, PWV pulse wave velocity, AIx augmentation index, ABI ankle-brachial index, ao aortic, br brachial, cf carotid-femoral
I unit increase in skin AF was associated with 46% higher OR for vascular stiffness when vascular stiffness was defined with a threshold of cfPWV ≥ 10 m/s (Fig. 3a) and 35% higher OR when vascular stiffness was divers with a threshold of cfPWV ≥ 12 m/s (Fig. 3b). No violation of linearity could be observed in the corresponding splines (Fig. iii).
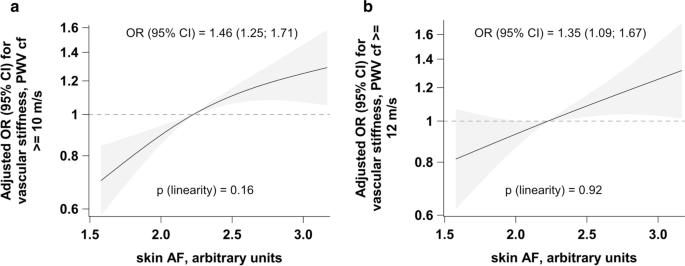
Adjusted odds ratios for relationships between skin AF and vascular stiffness. Adjusted associations between skin AF and vascular stiffness defined as cfPWV ≥ 10 m/south (a) and cfPWV ≥ 12 m/s (b). Linearity was assessed with Wald test from restricted cubic splines, adjusted ORs are reported from logistic regression and per 1 unit increase in skin AF. Analyses were adapted for sex and age, BMI, waist circumference, smoking condition (3 categories: non-smoker, former smoker, current smoker), recreational physical activity (biking and sports, h/week), systolic and diastolic claret pressure, pulse, prevalent atmospheric condition (prevalent heart failure, prior myocardial infarction or stroke), antihypertensive and lipid-lowering handling, CRP, LDL-, HDL- and total cholesterol, triglycerides and HbA1c. AF autofluorescence, cfPWV carotid-femoral pulse moving ridge velocity, OR odds ratio, CI conviction interval
Relationships betwixt skin AF and vascular stiffness across glycemic strata in the OGTT subset, north = 1348
Similar patterns of associations could exist observed for glycemic strata defined by either FPG or as "any aberrant glycemic parameter" on the one hand and those strata defined by either HbA1c or ii h plasma glucose on the other hand. The associations of peel AF with PWV and brAIx appeared to be much stronger in the prediabetes groups compared to normoglycemic groups when those groups were defined based on FPG or as "any abnormal glycemic parameter", Tabular array three. In contrast, the associations with PWV were not substantially unlike betwixt normoglycemic and prediabetes groups in the strata divers by HbA1c and two h plasma glucose levels. Yet, none of the interactions of skin AF with glycemic status in the OGTT subset was statistically pregnant. The estimates for ABI were consistent beyond all glycemic strata and definitions, with the exception of prediabetes group defined co-ordinate to 2 h plasma glucose levels, Table iii.
Discussion
This study demonstrates that AGE, measured as peel AF, were robustly associated with measures of arterial stiffness, such as PWV, AIx and ABI, independent of potential cardiometabolic confounders and glycemic status of the participants. The associations appeared to be more than pronounced in men and younger individuals. Furthermore, the relationships of PWV and ABI with skin AFseemed to be stronger than with several other classic risk factors for atherosclerosis such as CRP, HbA1c, and even age.
Our findings are consequent with earlier studies investigating the associations between Historic period, CVD, atherosclerosis and arterial stiffness in diabetes patients [9, 13, fourteen, 25]. Notwithstanding, in normoglycemic individuals, previous studies were inconclusive [9, 15, 16]. The discrepancies in these studies tin exist probably attributed to smaller sample size, measurement error, distinct measurements of vascular stiffness (PWV, AIx, pulse pressure, etc.) and Historic period (plasma or serum measurements of specific Age agents, skin autofluorescence) and differences in the composition (age, race, sex activity, etc.) of study populations. We demonstrate that the relationships between skin AF and vascular stiffness are not restricted to diabetic and prediabetic groups just are besides present in normoglycemic populations. Mechanistic studies suggest that Historic period promote endothelial dysfunction resulting in vasodilatory impairment [26], and diabetic and healthy individuals are on the whole every bit vulnerable to the deleterious effects of acute AGE load on vascular endothelium [4]. Both endogenous and exogenous AGE dilate the expression and release of vascular jail cell adhesion molecule-i [27, 28], increase production of reactive oxygen species and decrease NO bioavailability [3, 26], directly impacting endothelial cells and contributing to functional arterial stiffness. AGE modify ECM proteins in the vascular wall and may atomic number 82 to the germination of intermolecular and intramolecular crosslinks with collagen and elastin, triggering structural arterial stiffness [3]. As a result of glycation, modification of lipoprotein promotes foam cell germination. Interestingly, in the Epic-Potsdam cohort, HDL-, LDL- and full cholesterol all decreased across peel AF quintiles, even subsequently adjustment for lipid-lowering treatment.
Our written report is the offset to evaluate the relationships between skin AF and several aspects of vascular stiffening—reflected by PWV, AIx and ABI—beyond all glycemic strata and in ane setting. While aortic and carotid-femoral PVW is a proxy for big artery stiffness (arteriosclerosis), AIx was classically deemed a measure out of wave reflection intended to quantify the deleterious effect of systolic moving ridge reflection on cardiac workload, though its validity as a proxy for wave reflection magnitude has been questioned in recent studies [29]. ABI is an indicator of peripheral artery disease (PAD) progression, with nearly unremarkably used threshold ≤ 0.90 for diagnosis of PAD. Congruent with our findings that skin AF inversely associated with ABI, in a smaller clinical study performed in diabetes patients [xxx], plasma Age inversely associated with ABI, indicating that Age might contribute to the development of atherosclerosis in the beneath-the-genu peripheral avenue tree both in diabetic and normoglycemic populations.
Nosotros further observed an indication that, though the direction of the associations between pare AF and vascular stiffness was the same beyond all glycemic strata, the force of the relations may vary quite remarkably between normoglycemic and prediabetes participants, depending on the definition of prediabetes. Associations betwixt pare AF and vascular stiffness tended to be stronger in prediabetes groups based on FPG or divers equally any abnormal glycemic value compared to normoglycemic groups, whereas the relationships were not markedly different when prediabetes was based on HbA1c or 2 h plasma glucose levels. This finding is supported by a recent Mendelian randomization (MR) study investigating causal effects of prediabetes on major diabetes-related complications, including coronary artery disease (CAD) [31]. Intriguingly, while FPG concentrations were causally related to CAD with a 26% college odds of CAD per mmol/L increase in fasting glucose, no causal relationship between genetically elevated HbA1c levels and diabetes complications could exist detected in that written report. FPG has been shown to be causally related to vascular stiffness independent of genetically elevated gamble of type 2 diabetes in one study [32] and to subclinical atherosclerosis in individuals without diabetes in some other MR study [33], although no other glycemic parameters except FPG were evaluated there. Moreover, accumulating testify suggests that prediabetes stages defined past FPG (IFG) and two h plasma glucose (IGT) might have different pathophysiologies and consequences, thus representing fundamentally different metabolic conditions [34, 35]. IFG is characterized by reduced hepatic insulin sensitivity, stationary beta jail cell dysfunction and/or chronic low beta cell mass, contradistinct glucagon-likepeptide-1 secretion and inappropriately elevated glucagon secretion. In dissimilarity, IGT includes reduced peripheral insulin sensitivity, nigh-normal hepatic insulin sensitivity, progressive loss of beta cell part, reduced secretion of glucose-dependent insulinotropic polypeptide and inappropriately elevated glucagon secretion [34, 35]. A better understanding of the etiology and pathophysiological consequences of various prediabetic stages is the first step towards precision medicine in diabetes.
Birthday, these and previously reported information support the view that AGE might be involved in pathophysiological processes affecting vascular integrity and function, and preventive strategies targeting AGE aggregating, inhibiting AGE formation and interaction of AGE with their corresponding receptors (RAGE) appear as promising approaches to alleviate the Age burden on the progression of vascular stiffness. Inhibition of Age formation by aminoguanidine was shown to ameliorate arterial compliance in older humans with vascular stiffening [36]. Recently, Dna aptamers targeting Age–RAGE interaction have been developed, yielding encouraging results in experimental studies [37]. The use of alagebrium, an AGE-billow, was inversely correlated with plasma matrix metalloproteinase-9 and type 1 collagen, suggesting that this drug could also reduce the structural arterial stiffness [38]. Finally, lifestyle interventions such as smoking secession and dietary Historic period restriction could exist tested to reduce the chronic impact of exogenous Age on the vasculature [39].
Our study benefited from a large sample size in a low-run a risk setting, nested within population-based Epic-Potsdam study. Nosotros assessed different measures of arterial stiffness, which allowed us to perform comparative analyses and non to restrict our analyses to the relationships with PWV only. Exposures, outcomes and diverse cardiometabolic confounders were measured by trained staff using standardized protocols, and the study personnel were unaware of specific research questions of this study, minimizing observer and reporting bias. Finally, a substantial number of participants underwent an OGTT, facilitating a refined label of the relationships between AGE and vascular stiffness in various glycemic strata with differing affliction progression. Caveats include cross-sectional written report design, and because of observational nature of our study, a rest confounding cannot exist ruled out. Our written report population was primarily of older individuals of European beginnings, and the findings need to exist confirmed in other ethnicities and historic period groups. The accumulation of Historic period is a general characteristic of the aging tissue due to glycation and oxidation reactions. Nonetheless, we adjusted all analyses for age, thus, this factor is less probable to derange the results of this written report. Further, Historic period were measured merely in skin and not e.g. in plasma. Consequently, it was non possible to identify which AGE amanuensis was driving the observed relationships with vascular stiffness. Nosotros likewise could not study the interrelationships of skin-deposed Age with circulating AGE and soluble receptors for AGE (sRAGE) regarding vascular stiffening. Mayer et al. indicated that the ratio of pare AF and sRAGE might exist a more than sensitive parameter for the assessment of annual changes in aortic PVW than skin AF or circulating Historic period, because merely this ratio remained significant in the stepwise regression model [40]. Yet, in another report in patients with aortic stenosis, the ratio betwixt valvular AGE and plasma sRAGE was not statistically associated with the disease severity parameters such as aortic valve expanse in multivariable models, while valvular (tissue) AGE were significantly associated [41]. In comparative studies, the correlation between plasma and skin AGE was fairly moderate to skilful [42]. However, circulating Historic period are more prone to fluctuations due to dietary intake and excretion and therefore may not accurately reflect the long-term Historic period accumulation in tissues. Skin AF can be used in subjects with a peel pigmentation up to Fitzpatrick type 5 [ten]. It utilizes auto-fluorescent properties which sure dermal AGE such as pentosidine possess and has been validated with the Age content measured in skin biopsies [8]. Meerwaldt et al. showed a stiff correlation between skin AF measured with AGE-Reader and the fluorescent Age CLF and pentosidine likewise as the non-fluorescent AGE CML and Nε-carboxyethyl-lysine in the dermal layer of the skin, which were obtained from peel biopsies [8]. Moreover, Hofmann et al. found that skin AF strongly correlated with collagen fractions isolated from vein graft material by proteolysis and collagenase digestion and quantified by hydroxyproline assay, and both parameters correlated with PWV [43].
Since the AGE Reader™ uses light to detect Historic period, the measurements in individuals with a very night skin are difficult, due to absorption of both the incoming light and the fluorescent low-cal. Nonetheless, EPIC-DZD participants were exclusively of cardinal European origin with light skin. Some other limitation of the device is a potential interference of skin cream with pare AF measurements. Especially self-browning and sun blocker creams could block the incident light and crusade unreliable peel AF measurements. Of all participants, who underwent Age measurements, just thirteen participants reported using self-browning, dominicus blocker or other skin cream, and the median Age values in these participants were not different from those, who did not utilise whatever skin foam. Skin AF might prove useful every bit a rapid, not-invasive and toll-effective method to evaluate tissue Historic period accumulation in interventional studies.
Conclusions
In determination, in community-dwelling older adults, AGE measured by peel AF associated with measures of arteriosclerosis, wave reflection and peripheral arterial disease and appeared as an important correspondent to the evolution of macrovascular dysfunction independent of cardiometabolic confounders. The observed relationships were strongest in men and younger individuals and persisted beyond all glycemic strata.
Availability of data and materials
The datasets analyzed during the current study are not publicly bachelor due to data protection regulations. In accord with German Federal and Land data protection regulations, epidemiological information analyses of EPIC-DZD may be initiated upon an informal inquiry addressed to the secretariate of the Homo Study Eye (Part.HSZ@dife.de). Each request will then accept to pass a formal process of application and review by the respective PI and a scientific board.
Abbreviations
- ABI:
-
Talocrural joint-brachial index
- AF:
-
Autofluorescence
- Age:
-
Advanced glycation end-products
- AIx:
-
Augmentation index
- ao:
-
Aortic
- br:
-
Brachial
- BMI:
-
Body mass index
- CAD:
-
Coronary artery affliction
- cf:
-
Carotid-femoral
- CI:
-
Conviction interval
- CRP:
-
C-reactive protein
- CVD:
-
Cardiovascular affliction
- DBP:
-
Diastolic blood pressure
- ECM:
-
Extracellular matrix
- eNOS:
-
Endothelial nitric oxide synthase
- Ballsy:
-
European Prospective Investigation into Cancer and Nutrition study
- ESC:
-
European Society of Cardiology
- FPG:
-
Fasting plasma glucose
- HbA1c :
-
Hemoglobin A1c
- HDL:
-
High-density lipoprotein cholesterol
- IFG:
-
Dumb fasting glucose
- IGT:
-
Impaired glucose tolerance
- IQR:
-
Interquartile range
- LDL:
-
Low-density lipoprotein cholesterol
- MR:
-
Mendelian randomization
- NF-κB:
-
NF-κ light-chain enhancer of activated B cells
- NO:
-
Nitric oxide
- OGTT:
-
Oral glucose tolerance test
- OR:
-
Odds ratio
- PAD:
-
Peripheral artery illness
- PWV:
-
Pulse wave velocity
- SBP:
-
Systolic blood pressure
- VSMC:
-
Vascular shine muscle cells
References
-
Lacolley P, Regnault V, Laurent S. Mechanisms of arterial stiffening: from mechanotransduction to epigenetics. Arterioscler Thromb Vasc Biol. 2020;twoscore(5):1055–62.
-
Chirinos JA, Segers P, Hughes T, Townsend R. Large-artery stiffness in health and disease: JACC country-of-the-fine art review. J Am Coll Cardiol. 2019;74(ix):1237–63.
-
Goldin A, Beckman JA, Schmidt AM, Creager MA. Advanced glycation end products: sparking the development of diabetic vascular injury. Circulation. 2006;114(half dozen):597–605.
-
Uribarri J, Stirban A, Sander D, Cai Due west, Negrean M, Buenting CE, et al. Single oral challenge by advanced glycation terminate products acutely impairs endothelial function in diabetic and nondiabetic subjects. Diabetes Intendance. 2007;30(10):2579–82.
-
Chakravarthy U, Hayes RG, Stitt AW, McAuley E, Archer DB. Constitutive nitric oxide synthase expression in retinal vascular endothelial cells is suppressed by high glucose and advanced glycation end products. Diabetes. 1998;47(6):945–52.
-
Henaut L, Mary A, Chillon JM, Kamel Southward, Massy ZA. The impact of uremic toxins on vascular smooth muscle cell office. Toxins (Basel). 2018;ten(6):218.
-
Zhang D, Bi X, Liu Y, Huang Y, Xiong J, Xu Ten, et al. High phosphate-induced calcification of vascular polish muscle cells is associated with the TLR4/NF-kappab Signaling pathway. Kidney Blood Press Res. 2017;42(6):1205–15.
-
Meerwaldt R, Graaff R, Oomen PHN, Links TP, Jager JJ, Alderson NL, et al. Unproblematic not-invasive cess of advanced glycation endproduct accumulation. Diabetologia. 2004;47(7):1324–30.
-
van Eupen MG, Schram MT, van Sloten TT, Scheijen J, Sep SJ, van der Kallen CJ, et al. Skin autofluorescence and pentosidine are associated with aortic stiffening: the maastricht study. Hypertension. 2016;68(iv):956–63.
-
Koetsier M, Nur Eastward, Chunmao H, Lutgers HL, Links TP, Smit AJ, et al. Skin colour independent assessment of crumbling using pare autofluorescence. Opt Express. 2010;18(xiv):14416–29.
-
McNulty M, Mahmud A, Feely J. Avant-garde glycation stop-products and arterial stiffness in hypertension. Am J Hypertens. 2007;twenty(3):242–seven.
-
Utescu MS, Couture Five, Mac-Way F, De Serres SA, Marquis K, Lariviere R, et al. Determinants of progression of aortic stiffness in hemodialysis patients: a prospective longitudinal report. Hypertension. 2013;62(1):154–60.
-
Sell DR, Sun West, Gao 10, Strauch C, Lachin JM, Cleary PA, et al. Skin collagen fluorophore LW-1 versus peel fluorescence as markers for the long-term progression of subclinical macrovascular affliction in type one diabetes. Cardiovasc Diabetol. 2016;xv:30.
-
Saremi A, Howell S, Schwenke DC, Bahn K, Beisswenger PJ, Reaven PD, et al. Advanced glycation end products, oxidation products, and the extent of atherosclerosis during the VA diabetes trial and follow-up study. Diabetes Care. 2017;40(4):591–8.
-
Semba RD, Najjar SS, Sun 1000, Lakatta EG, Ferrucci L. Serum carboxymethyl-lysine, an advanced glycation end production, is associated with increased aortic pulse wave velocity in adults. Am J Hypertens. 2009;22(1):74–9.
-
Huang QF, Sheng CS, Liu Grand, Li FH, Li Y, Wang JG. Arterial stiffness and wave reflections in relation to plasma advanced glycation terminate products in a Chinese population. Am J Hypertens. 2013;26(6):754–61.
-
Henry RM, Kostense PJ, Spijkerman AM, Dekker JM, Nijpels G, Heine RJ, et al. Arterial stiffness increases with deteriorating glucose tolerance status: the Hoorn Study. Circulation. 2003;107(16):2089–95.
-
Gomez-Sanchez L, Garcia-Ortiz L, Patino-Alonso MC, Recio-Rodriguez JI, Feuerbach North, Marti R, et al. Glycemic markers and relation with arterial stiffness in Caucasian subjects of the MARK study. PLoS ONE. 2017;12(4):e0175982.
-
McEniery CM, Wilkinson IB, Johansen NB, Witte DR, Singh-Manoux A, Kivimaki M, et al. Nondiabetic glucometabolic status and progression of aortic stiffness: the whitehall II study. Diabetes Care. 2017;forty(iv):599–606.
-
Boeing H, Wahrendorf J, Becker Due north. EPIC-Germany—a source for studies into diet and gamble of chronic diseases European Investigation into Cancer and Nutrition. Ann Nutr Metab. 1999;43(4):195–204.
-
Nurnberger J, Michalski R, Turk TR, Opazo Saez A, Witzke O, Kribben A. Can arterial stiffness parameters be measured in the sitting position? Hypertens Res. 2011;34(2):202–8.
-
Teren A, Beutner F, Wirkner K, Loeffler Grand, Scholz M. Validity, intra- and inter-observer reliability of automated devices for the assessment of ankle brachial index using photograph-plethysmography. BMC Cardiovasc Disord. 2013;13:81.
-
Van Bortel LM, Laurent S, Boutouyrie P, Chowienczyk P, Cruickshank JK, De Backer T, et al. Skillful consensus document on the measurement of aortic stiffness in daily practise using carotid-femoral pulse wave velocity. J Hypertens. 2012;thirty(3):445–8.
-
Mancia Grand, De Backer Thousand, Dominiczak A, Cifkova R, Fagard R, Germano Chiliad, et al. 2007 guidelines for the management of arterial hypertension: the chore strength for the management of arterial hypertension of the European Social club of Hypertension (ESH) and of the European Lodge of Cardiology (ESC). J Hypertens. 2007;25(half-dozen):1105–87.
-
Koska J, Saremi A, Howell S, Bahn Grand, De Courten B, Ginsberg H, et al. Advanced glycation finish products, oxidation products, and incident cardiovascular events in patients with blazon 2 diabetes. Diabetes Intendance. 2018;41(3):570–6.
-
Bucala R, Tracey KJ, Cerami A. Advanced glycosylation products quench nitric oxide and mediate defective endothelium-dependent vasodilatation in experimental diabetes. J Clin Invest. 1991;87(2):432–viii.
-
Cai W, He JC, Zhu Fifty, Peppa G, Lu C, Uribarri J, et al. High levels of dietary advanced glycation cease products transform low-density lipoprotein into a strong redox-sensitive mitogen-activated protein kinase stimulant in diabetic patients. Circulation. 2004;110(3):285–91.
-
Basta 1000, Lazzerini M, Del Turco S, Ratto GM, Schmidt AM, De Caterina R. At to the lowest degree ii distinct pathways generating reactive oxygen species mediate vascular prison cell adhesion molecule-i induction past advanced glycation terminate products. Arterioscler Thromb Vasc Biol. 2005;25(7):1401–7.
-
Heusinkveld MHG, Delhaas T, Lumens J, Huberts W, Spronck B, Hughes AD, et al. Augmentation index is not a proxy for wave reflection magnitude: mechanistic analysis using a computational model. J Appl Physiol (1985). 2019;127(2):491–500.
-
Lapolla A, Piarulli F, Sartore G, Ceriello A, Ragazzi E, Reitano R, et al. Advanced glycation finish products and antioxidant status in type 2 diabetic patients with and without peripheral artery illness. Diabetes Care. 2007;30(3):670–vi.
-
Mutie PM, Pomares-Millan H, Atabaki-Pasdar Due north, Jordan Northward, Adams R, Daly NL, et al. An investigation of causal relationships between prediabetes and vascular complications. Nat Commun. 2020;11(1):4592.
-
Gottsater One thousand, Hindy Thou, Orho-Melander M, Nilsson PM, Melander O. A genetic risk score for fasting plasma glucose is independently associated with arterial stiffness: a Mendelian randomization study. J Hypertens. 2018;36(four):809–14.
-
Rasmussen-Torvik LJ, Li M, Kao WH, Couper D, Boerwinkle E, Bielinski SJ, et al. Association of a fasting glucose genetic risk score with subclinical atherosclerosis: The Atherosclerosis Risk in Communities (ARIC) written report. Diabetes. 2011;60(1):331–5.
-
Meyer C, Pimenta W, Woerle HJ, Van Haeften T, Szoke E, Mitrakou A, et al. Different mechanisms for impaired fasting glucose and impaired postprandial glucose tolerance in humans. Diabetes Intendance. 2006;29(8):1909–14.
-
Faerch K, Borch-Johnsen K, Holst JJ, Vaag A. Pathophysiology and aetiology of impaired fasting glycaemia and impaired glucose tolerance: does information technology matter for prevention and treatment of type 2 diabetes? Diabetologia. 2009;52(9):1714–23.
-
Kass DA, Shapiro EP, Kawaguchi Thou, Capriotti AR, Scuteri A, deGroof RC, et al. Improved arterial compliance by a novel advanced glycation end-product crosslink billow. Apportionment. 2001;104(thirteen):1464–seventy.
-
Yamagishi SI, Matsui T. Therapeutic potential of Deoxyribonucleic acid-aptamers raised confronting Age-RAGE axis in diabetes-related complications. Curr Pharm Des. 2018;24(24):2802–nine.
-
Zieman SJ, Melenovsky V, Clattenburg L, Corretti MC, Capriotti A, Gerstenblith G, et al. Advanced glycation endproduct crosslink billow (alagebrium) improves endothelial function in patients with isolated systolic hypertension. J Hypertens. 2007;25(3):577–83.
-
Yamagishi S, Matsui T. Pathologic office of dietary advanced glycation cease products in cardiometabolic disorders, and therapeutic intervention. Nutrition. 2016;32(ii):157–65.
-
Mayer O, Gelzinsky J, Seidlerova J, Materankova M, Mares S, Svobodova Five, et al. The office of advanced glycation end products in vascular crumbling: which parameter is the almost suitable as a biomarker? J Hum Hypertens. 2020;35:240–9.
-
Kopytek M, Zabczyk Yard, Mazur P, Undas A, Natorska J. Accumulation of advanced glycation end products (AGEs) is associated with the severity of aortic stenosis in patients with concomitant blazon ii diabetes. Cardiovasc Diabetol. 2020;19(1):92.
-
Liu CY, Huang QF, Cheng YB, Guo QH, Chen Q, Li Y, et al. A comparative written report on skin and plasma advanced glycation cease products and their associations with arterial stiffness. Pulse (Basel). 2017;four(4):208–18.
-
Hofmann B, Adam Ac, Jacobs Yard, Riemer M, Erbs C, Bushnaq H, et al. Advanced glycation end product associated skin autofluorescence: a mirror of vascular role? Exp Gerontol. 2013;48(i):38–44.
Acknowledgements
We thank the Human being Study Centre (HSC) of the High german Constitute of Human Nutrition Potsdam-Rehbrücke, namely the trustee and the information hub for the processing, and the participants for the provision of the information, the biobank for the processing of the biological samples and the head of the HSC, Manuela Bergmann, for the contribution to the study design and leading the underlying processes of data generation.
Funding
Open Access funding enabled and organized by Projekt Bargain. This work was supported past a Grant from the German language Ministry of Teaching and Research (BMBF) and the State of Brandenburg (DZD Grant 82DZD00302).
Author information
Affiliations
Contributions
AB and MBS designed the study and interpreted the data. AB performed statistical analyses and drafted the manuscript. RC, Atomic number 26, EP substantially contributed to interpretation of information and statistical analyses. All authors critically revised and approved the final manuscript. AB had full access to all data and takes responsibility for the integrity of the data and the accurateness of the analyses. AB and MBS are guarantors of the study and take full responsibility for the work and decision to publish it. All authors read and approved the last manuscript.
Corresponding authors
Ideals declarations
Ethics approval and consent to participate
The study was conducted co-ordinate to the Proclamation of Helsinki and approved by the Ethical Commission of the State of Brandenburg, Germany (S9/2002). All participants provided written informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional data
Publisher's Notation
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Effigy S1. Flowchart of inclusion. Tabular array S1. Mutually-adapted associations between skin AF and vascular stiffness in the Ballsy-DZD Written report.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits apply, sharing, adaptation, distribution and reproduction in any medium or format, every bit long equally you requite advisable credit to the original author(southward) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third political party material in this commodity are included in the article'southward Creative Eatables licence, unless indicated otherwise in a credit line to the material. If material is non included in the article's Creative Commons licence and your intended apply is not permitted by statutory regulation or exceeds the permitted employ, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Artistic Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/goose egg/ane.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and Permissions
About this article
Cite this article
Birukov, A., Cuadrat, R., Polemiti, E. et al. Advanced glycation end-products, measured as skin autofluorescence, associate with vascular stiffness in diabetic, pre-diabetic and normoglycemic individuals: a cross-sectional study. Cardiovasc Diabetol 20, 110 (2021). https://doi.org/x.1186/s12933-021-01296-five
-
Received:
-
Accepted:
-
Published:
-
DOI : https://doi.org/10.1186/s12933-021-01296-5
Keywords
- Advanced glycation terminate-products
- Age
- Ankle-brachial alphabetize
- Augmentation index
- Prediabetes
- Glycemia
- Pulse moving ridge velocity
- Pare autofluorescence
- Vascular stiffness
Source: https://cardiab.biomedcentral.com/articles/10.1186/s12933-021-01296-5
Posted by: petersonandere.blogspot.com

0 Response to "Can Advanced Glycation End Products Be Removed From Skin"
Post a Comment